Newsletter April 2023
Behavioral Health
Todd Lewicki, PhD, LMSW, MBA
Chief Behavioral Health Officer
Utilization Management & Care Coordination
Skye Pletcher-Negrón, LPC, CAADC
Director of Utilization and Care Management
Conflict-Free Access & Planning: Overview & Next Steps
OVERVIEW
The concept of conflict-free access and planning (CFAP), also known as conflict-free case management, requires that assessment and service planning are separate from the direct delivery of services, with the goal of objectively separating (or “firewalling”) potential assessment/eligibility/monitoring, direct service provision, and financial oversight conflicts a case holder or agency may have. A firewall is considered a legitimate way to keep financial interests separate between agencies paid to provide care. The intent of a firewall is that a single agency is not both assessing and identifying what services an individual needs and then providing those services to individuals. Presently, behavioral health services agencies allow the assessor to also provide services to the individual using “safeguards” against conflict. Safeguards are procedural practices intended to separate agency interests including for example, independent facilitation, self-determination, person-centered planning, fiscal intermediary, etc. Safeguards have generally not been regarded as adequate, but that there should be a combination of a firewall and safeguards to ensure full compliance with the strictest interpretation of CFAP. Presently, Michigan has largely
relied on the use of safeguards to mitigate potential conflict.
CFAP is codified in four federal policy initiatives: The Balancing Incentive Program within The Affordable Care Act (ACA); Community First Choice (CFC) within the ACA; Home and Community-Based Services (HCBS) Settings Final Rule (CMS 2249F) and The Older Americans Act Reauthorization Act. The Centers for Medicare & Medicaid Services (CMS) has been increasingly focused in recent years on ensuring that state Medicaid programs comply with federal CFAP requirements.
CFAP attempts to define where conflict in service arrangement exist:
- Providers responsible for evaluation, plan development, and direct service may have a financial conflict without adequate firewalls.
- Interest in keeping and serving an individual rather than promoting independence and autonomy.
- Service plans may focus on the convenience of the system, case holder, or service provider rather than a person-centered focus.
- Patterns of provider self-referral and undue influence may compromise individual choice of services or of providers.
- Inadequate oversight of the person-centered plan or quality of services.
The exception details to CFAP include:
- Exception given to regions without sufficient providers able to serve eligible populations.
- The state determines an exception is allowed.
- Regions granted exceptions must put protections into place, like as they have currently.
The authors of this article do not agree that safeguards in the current Pre-Paid Inpatient Health Plan (PIHP) and Community Mental Health Service Program (CMHSP) system are lacking in reasonable deterrent against conflict. However, to be compliant with federal policy, the state of Michigan feels it must demonstrate to the Centers for Medicare & Medicaid Services (CMS) that even potential conflicts of interest are mitigated or eliminated in Michigan’s public behavioral health system. The Michigan Department of Health and Human Services (MDHHS)
has not been cited by CMS regarding any specific conflict of interest.
To work toward a recommendation for compliance with federal CFAP requirements, the MDHHS convened a statewide CFAP Workgroup in early 2022, tasked with understanding federal CFAP regulations, evaluating current practices, and providing feedback on options for statewide implementation of additional protections and safeguards. The CFAP Workgroup is comprised of representatives from a variety of PIHPs and CMHSPs across the state (including several from the MSHN region), as well as consumer and advocate perspectives. The workgroup’s goal
was to provide input into strengthening protections against conflict of interest (especially financial) that would prioritize the individual’s experience using existing structures wherever possible.
The graphic below illustrates the CFAP Workgroup project plan and timeline for completion:
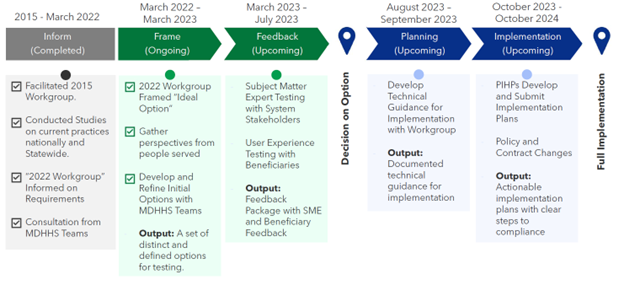
The stages involved learning more information on the CFAP requirements in the “Inform” phase. Next, moving into the “Frame” phase to define criteria and share perspectives on understanding CFAP. The “Feedback” phase begins a process of reviewing potential models and options for CFAP practice and testing each option. Once a recommendation on an option is made, MDHHS will develop technical guidance for the CFAP workgroup to use, and then lastly, the “Implementation” phase is intended for the PIHPs to develop implementation plans and include policy and contract changes. MDHHS expects this final phase to result in clear steps to compliance and full implementation by October 2024.
See full article for further information...
For any questions, comments or concerns related to the above, please contact Todd or Skye at Todd.Lewicki@midstatehealthnetwork.org or Skye.Pletcher@midstatehealthnetwork.org
